
Drug Information
Opioids are a class of drugs that include the illegal drug heroin, synthetic opioids such as fentanyl, and pain relievers available legally by prescription, such as oxycodone (OxyContin®), hydrocodone (Vicodin®), codeine, morphine, and many others. These drugs are chemically related and interact with opioid receptors on nerve cells in the body and brain. Opioid pain relievers are generally safe when taken for a short time and as prescribed by a doctor, but because they produce euphoria in addition to pain relief, they can be misused (taken in a different way or in a larger quantity than prescribed, or taken without a doctor’s prescription). Regular use—even as prescribed by a doctor—can lead to dependence and, when misused, opioid pain relievers can lead to overdose incidents and deaths. An opioid overdose can be reversed with the drug naloxone when given right away.Visit the National Institute on Drug Abuse for more information regarding Opioids.
Physical Signs
- Nausea
- Vomiting
- Itching
- Dry-mouth
- Noticeable elation/euphoria
- Confusion
- Slowed breathing
- Slowed heart rate
- Constricted Pupils
- Needle marks and bruising on an injection site
Other Signs
- Doctor shopping
- Shifting or dramatically changing moods
- Social withdrawal and isolation
- Other financial problems
Health Consequences
- Constipation
- Endocarditis
- Hepatitis
- HIV
- Addiction
- Fatal overdose
Opioid and Prescription Drug Misuse Prevention Resources
Naloxone

Prevention
Primary prevention activities are those directed at individuals who do not require treatment for substance misuse. For opioid use disorder, primary prevention involves reducing exposure and access to opioids, and reducing risk for developing an opioid use disorder among all age groups, including existing pain patients.
Talk to Your Physician
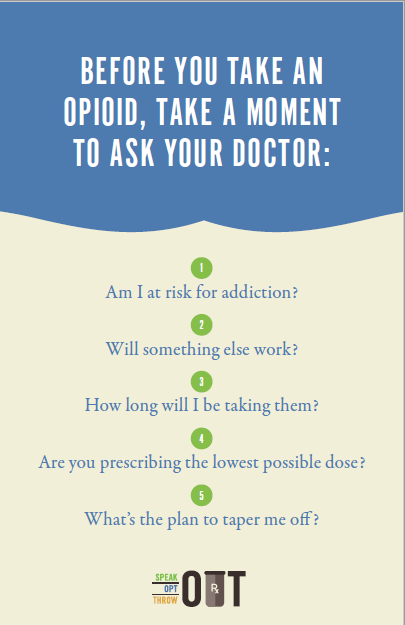
Before you take an opioid, take a moment to ask your doctor or dentist these five questions:
- Am I at risk for addiction?
- Will something else work?
- How long will I be taking them?
- Are you prescribing the lowest possible dose?
- What’s the plan to taper me off?
Properly Dispose of Medication
Proper disposal of opioid medications is important in curtailing the abuse of prescription drugs by reducing access to unused, unwanted or expired medications. It also reduces the negative impact on the environment. Safely dispose of your leftover or expired opioids by using a prescription drug drop box. Find a take-back location near you by using our search tool.
Understand Risk & Protective Factors
Addressing risk factors early and paying careful attention to children at higher risk can reduce that child’s likelihood of a future problem. This is a simplified list of some overall risk factors. Learn more at youth.gov
- Family history of substance use disorders
- Mental health or behavioral issues
- Trauma
- Impulse control problems
Protective factors may reduce the risk of youth engaging in substance use. Increasing protective factors in addition to reducing risk factors can be more effective in preventing substance use.
- Ability to make friends and get along with others
- Reliable support and discipline from caregivers
- Mastery of academic skills (math, reading, writing)
- School Engagement
These are simplified lists of some overall risk and protective factors. Learn more at youth.gov
Talk to Youth about Opioid Misuse
Children who learn about the risk of drugs at home are less likely to use drugs than those who do not get that critical message from their parents. Here are a few resources for getting the conversation started:
Naloxone Information
- Naloxone temporarily reverses an opioid overdose by blocking the brain’s opioid receptors, allowing breathing to be restored.
- The duration of the effect varies, but typically lasts between 30 and 60 minutes. After the opioid receptors are no longer blocked by Naloxone, the individual may resume overdosing. It is important to call 911, even if it appears that the individual is no longer overdosing.
- Naloxone only temporarily reverses overdoses due to opioid prescription pain relievers (such as Oxycontin and hydrocodone) and heroin. Administering Naloxone to someone overdosing on other drugs will not have an effect.
- In Idaho, anyone with a valid reason can ask for a prescription for naloxone from a physician, physician’s assistant, nurse practitioner, or pharmacist. The naloxone does not need to be intended for your own use. Someone who administers naloxone to a person who appears to be experiencing an opioid overdose is legally protected by Idaho’s Naloxone Access Law and Idaho’s Good Samaritan Law.
For more information on Naloxone and how to find Naloxone in your community, visit www.prevention.odp.idaho.gov/naloxone
NARCAN training video
Instructions for administration of NARCAN® Nasal Spray 4mg
Naloxone Videos
In English: Nasal
En Español: Naloxone Injectable | Naloxone Nasal
Policy
Non-prescription opioids, such as heroin, are Schedule I drugs meaning they have high potential for abuse and are not approved for medical use. Prescription opioids, including codeine, morphine, and hydrocodone, are Schedule II and still have a high potential for abuse but are approved for medical use with a prescription and further limitations.
Recent Idaho Legislation
Prescription Drug Monitoring Program
2015: House Bill No. 4
Requires prescribers to register with the state prescription drug monitoring program. Enacted March 5, 2015.
2017: House Bill No. 5
Requires pharmacists to register with the state prescription drug monitoring program. Enacted February 16, 2017.
Naloxone Access
2015: House Bill No. 108
Allows prescribers and pharmacists to prescribe opioid antagonists to a person at risk of experiencing an opioid-related overdose; a person in a position to assist a person at risk of experiencing an opioid-related overdose; a person who, in the course of his official duties or business, may encounter a person experiencing an opioid-related overdose; or a person who in the opinion of the prescriber or pharmacist has valid reason to be in the possession of an opioid antagonist. Allows these persons, when acting in good faith and exercising reasonable care, to administer an opioid antagonist to another person who appears to be experiencing an opioid-related overdose. Requires the administering person to contact emergency medical services as soon as possible. Ensures said persons will not be held civilly or criminally liable. Enacted March 23, 2015.
2019: House Bill No. 12
Amends existing law to revise provisions regarding opioid antagonists. Addresses use of the phrase “prescriber or pharmacist” in previous legislation creating concern among hospitals and other health professionals about their ability to prescribe and dispense naloxone. Replaces “prescriber or pharmacist” with “health professional licensed or registered under this title.” Signed by the Governor on February 14, 2019.
Good Samaritan Law
2018: House Bill No. 649
Adds a new Idaho Code Section 37-2739c to provide that certain persons acting in good faith seeking or needing medical assistance for drug related overdose shall not be charged or prosecuted for possession of controlled substances or drug paraphernalia. This Good Samaritan legislation shall not be grounds for suppression of evidence in other criminal charges. Enacted March 26, 2018.
 Official Government Website
Official Government Website